“In my country, this would not be possible. This could literally not happen.” – Student, Health Informatics, George Brown College, Toronto
As guest lecturers, we heard variations of this many times during and after our presentation about mindenpaper.com, our advocacy effort borne from Haliburton Highlands Health Services’ (HHHS) closure of the Emergency Department (ED) in Minden, Ont. Our audience consisted of many with extensive health-care experience, including dentists, pharmacists, nurses and people who run surgical teams.
We were floored each time we spoke with someone new. They were, too.
Only six weeks’ notice before an ER closure? How? How could this happen? In Canada – Why?
Before HHHS decided to close the Minden ED with just six weeks’ notice, few in Minden would have believed that international health-care professionals/students would view our town as an example of Canada’s health-care challenges.
Now, there’s a steadily increasing number of residents in Minden and surrounding areas who realize that our health-care system is spiralling out of control, and Minden might be a microcosm of the whole thing.
Our team, Minden Paper, has been passionately engaging with people and seeking the return of Minden ED, along with accountability and transparency from the HHHS board. The closure of the ED has become a rallying point for us to address broader issues affecting health-care systems nationwide.
It has allowed us to explore HHHS’s fiscal management, especially during the fiscal year 2023 (FY 23), and to express the urgent need for a province-wide examination of health-care system Chief Executive Officers (CEO) and board performance to determine the current situation and help make informed decisions moving forward.
At George Brown College, we discussed the ethos of mindenpaper.com, the influence of social determinants of health on our analysis to date, and board governance’s impact on the Minden closure. We explored our experiences since the April 20 announcement right up to that moment in class.
However, one thing we did not talk about was the criticality of labelling the x-axis/title when reverse-coding a deficit.
… If you’re reverse-coding a deficit, you need to label your x-axis/title on the chart
Those “reverse-coding a deficit” conversations came up separately, in chats with people who were looking to HHHS’s financial statements to try to ascertain the circumstances of the closure. Specifically, we had started talking with people who wanted to visualize FY 23 based on an analysis of the organization’s Financial Statements and Board Meeting Minutes, amongst other publicly available data.
When you’re talking about reverse coding a deficit for data visualization with people who take their inputs and outputs as seriously as a heart attack, you’re entering the upper echelon of a very particular domain. A world of complexity and precision. Accountability and responsibility. Stakeholder engagement. Continuous learning and adaptability. Ethics and integrity.
A world that is, in our opinion, incredibly analogous to health-care system fiscal management as we’ve come to understand it. Think about it:
The work of data visualization is intricate. It requires meticulous attention to detail to ensure clarity and accuracy in communicating data points, trends and narratives every step of the way. Fiscal management, even in the enormously complicated sense of operating a health-care system, shares these same traits.
Except, beyond the mere numbers and budgets, fiscal management has a profound effect on the lives of individuals and communities. Like the intricacies of data visualization, every step in health-care decision-making demands meticulous attention to detail, accountability and principled approaches.
Just as a mislabeled axis can lead to misinterpretation in data visualization, fiscal management challenges can lead to decisions that have tangible effects on individuals, households and communities, along with entire sectors and industries. The effects can be multigenerational – ask anyone from Fort Erie.
And so, it was with this understanding of what’s at stake that we joined financial analysts in trying to comprehend the larger nuances of health-care fiscal management at HHHS in hopes of understanding both the local and broader challenges facing our health-care system.
Overview
The management of HHHS is a joint effort between the CEO and the Board of Directors. Together, they develop a mission statement outlining HHHS’s main objectives, which might include refining services or exploring new areas. This mission translates into a detailed roadmap with specific, measurable milestones. While both the CEO and the board share responsibilities, each plays distinct roles to guarantee the organization’s success.
The CEO handles HHHS’s daily operations, ensuring it meets performance standards and financial benchmarks. If problems arise, the CEO addresses them and, for bigger challenges, collaborates with the board to find solutions.
The board provides oversight, ensuring HHHS aligns with its mission and achieves set goals. It prioritizes financial performance, including staying within approved budgets and ensuring stable cash flows.
The Ministry of Health (MOH) sets fiscal guidelines for HHHS. Though not involved in daily activities, MOH standards significantly influence HHHS’s financial management, demanding transparency and alignment.
In Ontario’s health-care system, the CEO and the board’s financial responsibilities determine the system’s sustainability and effectiveness. The CEO, often collaborating with the Chief Financial Officer, presents financial updates, addressing any deviations or opportunities. CEOs also connect with various external entities like governmental funders and donors to communicate the institution’s financial status and needs.
The board, on the other hand, supervises financial operations and holds the CEO accountable for the institution’s fiscal health. It plays a crucial role in budgeting, reviewing, questioning and endorsing the budgets, ensuring alignment with long-term goals. It also drafts financial guidelines, assesses fiscal threats and ensures risk mitigation strategies are in place. For transparency, a subset of the Board, typically the finance committee, works with external auditors to validate the organization’s financial statements.
While the CEO focuses on daily operations, the Board has a broader perspective, setting large-scale financial objectives in line with the mission and societal demands. Understanding this role distinction is vital as we delve into FY 23 fiscal management at HHHS.
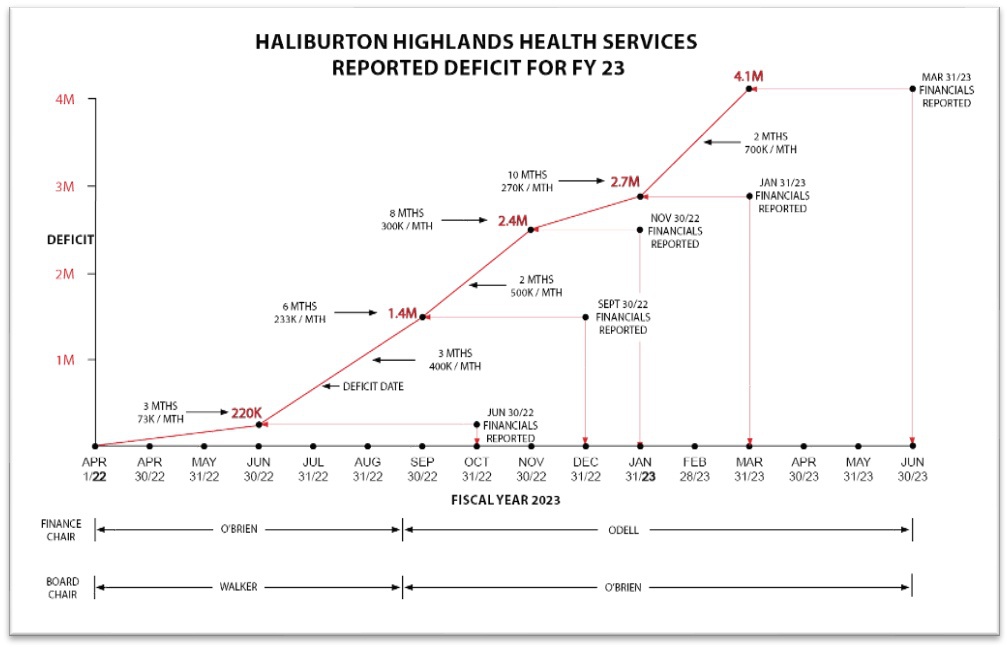
The numbers reflected on the HHHS Reported Deficit for FY 23 chart for the year ending March 31, 2023, are obtained from the posted minutes on the HHHS website.
- On June 30, 2022, financial statements showed a $220,000 deficit, which was reported on Oct. 27, 2022. The deficit averaged $73,000 monthly over April, May and June.
- The deficit was understated by $224,000 due to gains from property, buildings and equipment sales. The adjusted average monthly deficit was $148,000.
- On Sept. 30, 2022, financial statements showed a total deficit of $1.4 million, which was reported on Dec. 22, 2022. The deficit averaged $400,000 monthly over July, August and September.
- On Nov. 30, 2022, financial statements showed a total deficit of $2.4 million, which was reported on Jan. 26, 2023. The deficit averaged $500,000 monthly over the two months covered in that statement.
- On Jan. 31, 2023, financial statements showed a $2.7 million deficit, which was reported on March 23, 2023. The deficit averaged $150,000 monthly over December and January.
- The year-end deficit on March 31, 2023, was anticipated to be $3 million, as mentioned in the March 23, 2023, minutes.
- Audited financial statements presented at the Annual General Meeting on June 22, 2023, reported a $4.1million deficit for the fiscal year ending March 31, 2023.
- The average monthly operating deficit for the final two months of the fiscal year was $700,000.
- After removing gains on sales, the average monthly operating deficit for the fiscal year ended March 31, 2023, was $360,000.
Questions
- Why such fluctuations in the monthly deficits?
- Why the big jump in deficit in the audited financial statements?
- Regarding Note 21 from the financial statements: why could HHHS not estimate the additional monies to come?
- What was done to rein in the increasing deficits?
- Were there discussions with various stakeholders to get their input on controlling the deficits?
- Does the FY 24 budget show continued deficits?
- Where on the chart timeframe was the decision made to close Minden?
- Were the 2024 budget numbers available when the decision was made?
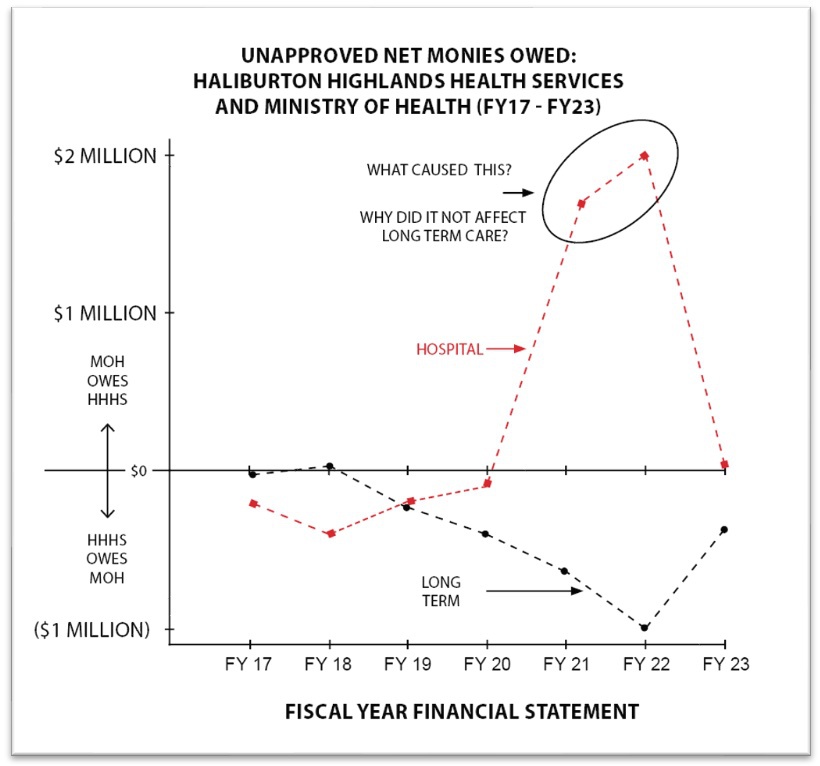
The numbers reflected on Unapproved Net Monies Owed: Haliburton Highlands Health Services and Ministry of Health (FY17 to FY23) are obtained from the audited financial statements posted on the HHHS website. In the “Notes” section of these financials, there is a schedule of these monies that is broken out by the various operating grants. The net amounts of monies recoverable (owed to HHHS) and refundable (owed by HHHS) for the hospital and the long-term care were obtained from these schedules and charted accordingly.
Questions
- What could cause such a significant increase in monies owed to HHHS in FY21 and FY22?
- Why is the trend only with the hospital and not LTC?
- What changed in FY23 that eliminated the trend?
- Are these reported “owed monies” included in reported revenue for the applicable fiscal year?
- If monies owed by MOH are not included in fiscal year revenue they are claimed for, when are they recorded as revenue?
- Do monies owed to the hospital that are claimed get changed by MOH?
- If yes to 6, where does that get reflected in future fiscal statements?
The numbers, graphs and fiscal details featured herein reveal a complex tale of hardship at HHHS – one that ultimately led to an unprecedented six-week timeframe for the closure of an Emergency Department that stood for nearly 30 years.
Do we know how many of our hospitals might be at risk of having the same outcome of closure?
It’s not just about numbers. Every fiscal challenge, every critical detail, translates into tangible health-care outcomes for real people – our families, friends and communities. The astoundment of our international peers and the passionate, powerful voices from our community indicate what we believe is a pivotal moment for change in Canadian health care.
As patients, residents and communities, we must demand clarity, accountability and a commitment to the highest standards of care. Minden’s experience must serve as a nationwide warning: review the financial management and board governance of your local health-care systems.
And don’t forget: Patients, residents, and community members were not consulted before, during or after the closure of the Minden ED.
Health-care systems nationwide can – and should – learn from that, too.
The authors would like to thank Anna Foat, Laura O’Grady and the people of Minden for their time and insight.


The comments section is closed.
Wonderfull article Jeff would you join our Yellowshirtbrgd or facebook Yellow Shirt BRIGADE Fort Erie and post it there. Thankyou in advance ☺️ Joy
Absolutely – thanks Joy hope you’re well!