The COVID-19 global pandemic has led to many paradigm shifts in the delivery of healthcare.
Virtual care is probably the most visible and stark change. Overnight, Canadian healthcare transformed itself from a heavy reliance on face-to-face encounters to a majority of interactions occurring via secure videoconferencing or telephone support, accelerating a change that had been years, if not decades, in the making. Now, most feel virtual care is here to stay.
But there is another change requiring a paradigm shift that has not yet happened: how Ontario funds hospice care.
Palliative and hospice care are often used synonymously and interchangeably. For clarity, palliative care is the umbrella term that refers to the care provided to patients with a life-threatening illness, preferably from the time of diagnosis (when resources permit) until end of life. Hospice care is synonymous with end-of-life care. This typically occurs in either a residential hospice or a patient’s home. Some residential hospices have community outreach programs that provide home hospice care with the residential hospice available as a backstop.
Residential hospices are built through philanthropic giving and fundraising. While the government partially funds the clinical operation of hospices, it is estimated that more than 50 per cent of the overall operating expenses must be raised year after year to make up for shortfalls. Hospices also rely heavily on volunteers, who are the lifeblood of hospices. From direct patient care to housekeeping, from meal preparation to night vigils, hospices simply do not function without their armies of care, their “caremongers.”
Hospices survive due to the generosity of their communities and the unfailing commitment of staff. The COVID-19 pandemic has exposed many shortcomings in our healthcare system and our funding of hospices is no exception. Donations have slowed to a trickle and it is unclear when fundraising activities will be able to resume. Even then, it is uncertain if fundraising will continue at pre-COVID levels given record unemployment and significant losses in the markets. Many volunteers are no longer able to support hospices due to the risk posed by their age or medical conditions. While some volunteers may be able to return in time, there is a very real possibility that most hospices will need to adjust to life without the irreplaceable volunteers.
In no other area of medicine would we tolerate this level of uncertainty and lack of support. Imagine a patient being told their chemotherapy or surgery was delayed or unavailable due to a slow year in fundraising.
While many hospitals run charitable foundations or charge for parking to supplement new capital expenditures, such as an MRI scanner or robotic surgical assistive device, day-to-day costs are fully funded through global budgets. It is estimated that residential hospices must fundraise almost $150/patient/night to make ends meet. Hospices pride themselves on providing their services “free of charge” to patients and their families. Now imagine the added costs of PPE required in the “new normal” of the pre-vaccine COVID reality that has decimated hospices financially and diminished their human resource base.
Hospices often sweat at year end, hoping that donations and philanthropy will make up for the shortfalls in government funding. Due to increased staffing and PPE costs combined with decreased donations and fundraising activities, the expected revenue losses for hospices in 2020 and going forward is eye-watering.
This underfunding of hospices flies in the face of our current economic understanding of the benefits of palliative care. In May 2020, Palliative Care Australia and KPMG released a report highlighting the need to not only overhaul the palliative care system in Australia but also make significant investments to realize cost savings.
According to the report: “All Australians who need palliative care are simply not having access to services when they need to, particularly at home and in community settings. As we prepare for an ageing population and other unexpected stresses to our health care system, like COVID-19, we must look seriously at reforming our system to ensure it can meet people’s needs into the future. Palliative care is about quality of life, living well with a palliative diagnosis and about dying well. Through an additional annual investment of $365 million on national reform, we can save up to $464 million in other health system costs while making the system work best for those experiencing it. We have to spend money to save money and that’s backed by leading economists” (emphasis mine).
These findings can be generalized for the Canadian context. We need to invest money in order to save money. To their credit, HPCO’s 2020 pre-budget submission to the provincial government recommended investments but also contained many “cost-free” recommendations for improving the efficiency and quality of hospice palliative care in Ontario.
Furthermore, Dr. Sandy Buchman, the president of the Canadian Medical Association and a palliative care physician, recently presented a slide at a ChoosingWisely conference that outlined the cost of care based on location of care. Here is what it showed:
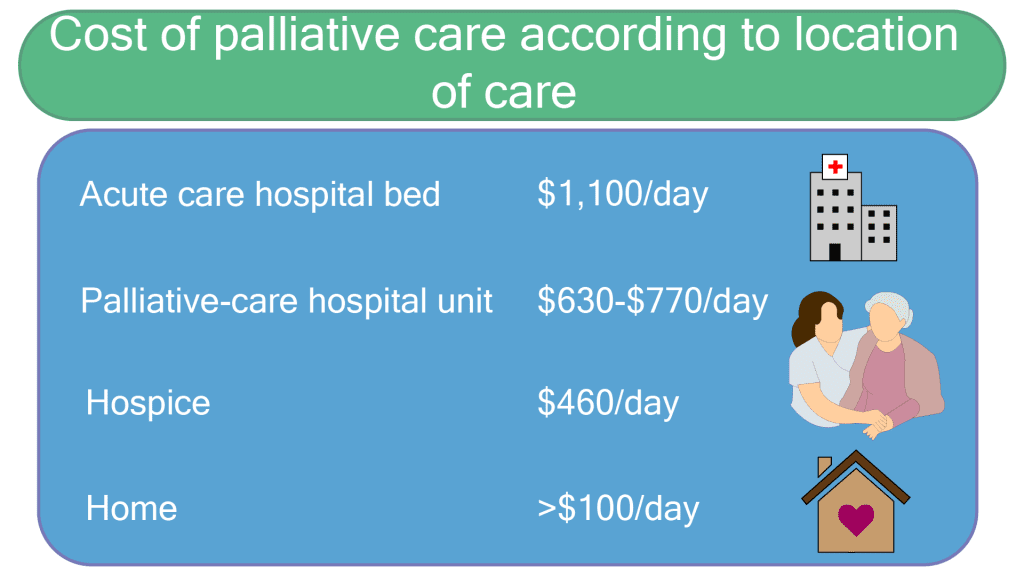
Clearly hospice care, whether at home or in a residential hospice, is more economical than providing the same care in hospitals. But we can’t do this if hospices are constantly fighting to keep their doors open and the lights on.
This pandemic threatens hospice care in Ontario. The time has come for the government to work with its partners and re-examine how we fund hospice care. We must ensure that hospice care will continue to be available to support patients and their families when they need it.


The comments section is closed.
Please note the lowest cost of all is for home hospice care currently, though it is a bare bones operation desperately in need of proper funding for full services. The burden falls foremost on home care-giving family members’ physical, emotional and mental health for their 24/7 unpaid care. This often necessitates taking leave from work temporarily or permanently and the emotional and financial toll does not end at time of death of the family member. The burden secondarily falls to the army of poorly paid and under-benefitted front line PSWs, the majority of whom are non-white and women, with the implicit racism in this apparent cost savings. In addition, the heavy reliance on volunteers for work that should be done by paid workers is now exposed by the new realities of this time.
Thanks Diane.
No arguments here. I work in both residential and community hospice. What you describe is reality.
Thank you Dr. Cargill for your eloquently written article highlighting the significant shortfalls that threaten our ability to provide a dignified end of life experience in Ontario. All of us that provide Palliative Care Support know that palliative care is good quality, economical care. Not only do we need to find an improved model for the funding of Hospice Care I would suggest we need an equal overhaul to the funding of the human resources required to continue to care for our dying neighbors in their own homes as is the wish of most Ontarians. Why are the home visiting Palliative Nursing and Personal Support workers the lowest paid in their domain of care? How can we expect these providers to remain committed to patients at home when they would receive better hours, pay and benefits if they were to work in more expensive institutions such as the acute or Long Term Care setting?
I will happily share your article to highlight the important issues you raise broadly!!
Thank you Racheal. Great point, the OMA Section of Palliative Medicine actually makes this argument as well. It is difficult to recruit and retain trained HCPs into palliative care when the positions are poorly remunerated. I refer it to it as a “benign neglect.” Since HCPs in palliative care rarely complain, it is assumed we are “ok” when we are clearly not.
I have an article coming out soon with Healthy Debate about physician human resources. Perhaps you would consider an article for Healthy Debate in the future as well?
This should be fully funded by our governmental health care system, as something that the public needs, as much as they need emergency care. Interesting how much effort, read that ‘expense’, is put into saving one’s life, yet when life is at the ultimate end, there are limited provisions made for the management of the process of dying. We, the public need to get more vocal and call on our government to revisit this imbalance.
Thanks Heather. Agree, public support would go a long way towards making this shift. For decades, they have subsidized hospice palliative care through their generosity. The time has come to reward that generosity.
Hospice is a wonderful caring place for people suffering from life threatening illnesses . The staff and volunteers do such a fantastic job caring for their patients in a homelike environment . We must ensure Hospice is kept going so many would lose out on the Hospice caring experience.
Thanks Janice. I agree. Sadly, most research shows that access to palliative care is getting worse, rather than better. Residential hospices are part of that puzzle.
Thank you for the excellent article.I agree with your call to action.
Thanks Lana. It is a call to action. Kind words and platitudes won’t keep the doors open. This requires commitment to action and follow through.
This is something that should concern everyone. At some time in some way we will all be in need of palliative care.
Precisely Theresa. Everyone can benefit from palliative care, whether it is advance care planning, cancer pain management or end of life care.
Then why is it treated like a health care luxury?
We need to provide in-home support to keep palliative patients at home with their families. Many years ago I looked after my mother-in-law in our home in the country just outside of Toronto. At the time, Ontario had an amazing home are program that provided a hospital bed, visiting nurse and doctor and respiratory support t9our home at no cost to us. This allowed us to be able to look after her and provide her with comfortable care to her death. Please bring back this more humane and much less costly care.
Thanks Linda.
Sadly, HQO recently reported that access to community based palliative care has stalled after “modest” improvements in 2016. Clearly more needs to be done.
My late husband entered Ruddy Shenkman hospice on June 22, 2019 where he received the best care possible. The Doctors, nurses and volunteers were exceptional. He survived for 7 weeks in the most beautiful surroundings, his bed was even wheeled out side overlooking the garden. This type of end of life establishments are a necessity and should be fully funded by the government. Our family is very grateful that he was able to spend his last days with a such compassionate group of people.
Thanks for making the case for adequate funding for hospice care Darren, not only because of the solid economic arguments, but also because it appropriately addresses people’s healthcare needs at the end of life. Interestingly, the figures quoted in the slide come from the Ontario government itself. This data was taken from the report of the Auditor General of Ontario in December 2014, the most recent report on palliative care. They know the economic argument well, and as you say they also know that they have to spend money to save money, but have continued to underfund because of a lack of political will to spend the upfront money required. Our system has always depended on the good will of donors and volunteers, and they know that this will continue so it lets them off the hook. But should this essential and appropriate healthcare always be dependent on charity? Especially with the extreme challenges that the pandemic has created? As you note, no other essential care in our “universal” healthcare system uses this charitable model exclusively. Fortunately, to the Ontario government’s credit, they now provide capital funding of $200K/bed for up to 10 beds to a maximum of $2M for new residential hospice construction. It’s a step in the right direction. Perhaps there is some light at the end of this very long tunnel. .
I am not going to argue with the CMA President and Freeman Chair for Palliative Care at North York General Hospital, lol.
There is a light at the end of the tunnel. Now, let’s turn it up a bit.
Imagine the benefits of applying the economics of palliative care to every patient facing a life-limiting illness in their last years of life, rather than last few months.
Now, imagine if we did it right from the time of diagnosis.
Better patient care AND better use of health care dollars.
Hospices play a key but underappreciated role in our health care system. They have much to offer.
Congratulations on your approval yesterday! A great accomplishment for your community.
Thanks Darren. And to your point about the economic benefits of palliative care right from the time of diagnosis, I’m working with Choosing Wisely Canada on an idea to promote and amplify ACP and these economic benefits is one of the core reasons. Stay tuned.
Thanks Brenda.
I’m glad to hear your experience with hospice was a positive one.
Thank you for mentioning volunteers. They are the lifeblood of hospice.
This is very important observation which challenges hospice and palliative care organizations to re-examine service delivery in the light of emerging new trends poised by Covid-19. Particularly the area of funding, it is a high time that hospice and palliative care should be fully supported by government. Especially now that the benefits can be clearly demonstrated.Goverment should be held responsible to provide hospice and palliative care.
Good morning,
Thank you for these reflections. As a current board member at Hospice Renfrew, I totally agree with your call to action. Surely our provincial ministries will see the light and recognize that properly funding residential hospices is a win-win financially and investing taxpayer dollars wisely will benefit all.
Donna Anderson
“Surely” :)
Thanks Donna, here’s hoping.
There is an election in 2022. Let’s hope full funding for hospices makes the platform of the successful party, if not funded sooner.
Thanks Paul. The benefits are HPC are undeniable. The KPMG study is one of many that highlight the need to “invest to save.” Care provided in the last 1-2 years of life is often the most expensive care for patients in our publicly funded system and while the goal of HPC is not cost savings, it is a “beautiful side effect.”
Thank you for this article- so hope that funding can be adjusted for these difficult times. I worked in Hospice Palliative care for 20+yrs and know first hand how vital the care is for patients , families and friends.
Thanks Marg for your dedication to HPC. While this model may have made sense decades ago, this is medically necessary care that should be appropriately funded and resourced.
Looking forward to questions, comments and gratuitous insults.
Time we do fund our hospice services and care! Well written. Thanks
Great article, Dr. Cargill! I’m a member of the board of directors at Hospice Wellington. Are you aware of any specific advocacy actions being undertaken here on Ontario to effect policy changes? I haven’t seen much from HPCO, but I may be looking in the wrong places.
Hi Joan,
I know HPCO works very hard on this behind the scenes.
Our best advocates, however, will always be our patients and families.