In the winter of 2015, James Hilgreen, a 41 year-old man from New York, kicked an old habit– one that millions of people around the world have been trying to beat for years. Hilgreen started smoking at the age of 18. He told news outlet CNN that he had tried using patches, gum and nicotine spray to quit, but failed each time. It was only with the use of e-cigarettes (vaping) that he finally found success.
Four years later, just over 900 miles west, Adam Henreder, a 17 year-old from Illinois, was hospitalized for one month in the intensive care unit with e-cigarette and vaping associated lung injury (EVALI). He had never previously used tobacco and started vaping to “fit in.” He was unaware of any health risks when he started using e-cigarettes and is now an advocate to prevent their use.
Governments around the world are struggling to determine the appropriate stance on e-cigarettes. Several countries have banned their use or sales, while some, including the UK, still promote vaping as a means of smoking cessation.
Stories on either side of the spectrum, like that of Hilgreen and Henreder, are what dominate media coverage of e-cigarettes. But it is important that we dig deeper to determine the proven risks, benefits, and remaining unknowns, before we can make an informed decision regarding their use.
Do e-cigarettes have any potential benefits?
Proponents say that e-cigarettes can help people quit smoking. This is based on a randomized controlled trial of 900 people receiving behavioural support treatment, which found that e-cigarettes increased quit rates from 9% to 18% in comparison to other methods of nicotine replacement (such as patches, gums and lozenges). In the UK, public health officials estimate that e-cigarettes help roughly 20,000 people quit smoking every year. In the US, Hilgreen is one of an estimated three million people who have replaced cigarette smoking with vaping. And in Canada, roughly one third of smokers report using e-cigarettes in a quit attempt within the past two years.
These results are important, given the magnitude of worldwide cigarette use and its associated harms. Over one billion people use cigarettes worldwide. Cigarettes are believed to be responsible for 70% of all lung cancers. People who smoke die, on average, 10 years before those who don’t. And most dishearteningly, combustible cigarette use leads to over 7 million deaths per year.
John Newton, director of health improvement at Public Health England, said to CNN, “if you smoke, there is no situation where it would be better for your health to continue smoking rather than switching completely to vaping.”
But it might be more complicated than this. Does the evidence really support e-cigarettes being safer than combustible ones? While many people assume that vaping is less harmful than smoking, that data simply isn’t available. Additionally, research shows that the vast majority of people who use e-cigarettes for smoking cessation will continue to use them indefinitely, making it all the more important to determine their long-term safety.
Public Health England released a highly contested statement earlier this year, suggesting that vaping was 95% safer than smoking cigarettes. But this claim was based on the fact that e-cigarettes have fewer chemicals, by quantity, without any evidence of how these chemicals interact with the body over time.
“The hypocrisy of calling this harm reduction based on a chemical analysis is that for everything else, we demand evidence, we demand randomized trials, and [here] we don’t even have observational data,” says Dr. Samir Gupta, a lung specialist physician and researcher at the University of Toronto. “We have no studies of long-term effects, and I am definitely worried. Many of the vape ingredients are things that are in cigarette smoke and known to be harmful. It will be five to 10 years or more before we have the data, and of course, by then it will be too late.”
Dr. Theo Moraes, a pediatric lung specialist at SickKids Hospital, references a stark analogy put forward by a World Health Organization bulletin. “If you’re a smoker, it’s like climbing to the 100th story of a building and jumping off. You know it’s going to be bad. If you’re an e-cigarette user, you’re jumping out of a window, you just don’t know what story you’re on.”
E-cigarettes and lung damage
Over 2,200 people in the US have been diagnosed with EVALI. And 47 Americans have died. A report in the New England Journal of Medicine described 53 detailed cases of EVALI in Illinois and Wisconsin, in which patients developed respiratory and gastrointestinal symptoms associated with the use of vaping nicotine and/or THC. Most patients were very sick, with roughly one in three requiring an intensive care unit. What’s worse, most of the patients were young and otherwise healthy.
Several researchers have suggested that vaping THC oil is responsible for acute lung injury. Henreder, like 84% of patients who developed EVALI in the NEJM study, self-reported that he vaped THC. Recent research from the CDC of lung fluid samples from 29 patients has identified Vitamin E acetate as the potential culprit. Vitamin E acetate is a synthetic form of vitamin E, used as a thickening agent in illicit THC oil and was not detected in the nicotine cartridges sampled.
However, the safety of non-THC containing e-cigarettes has also been called into question. Dr. Matthew Stanbrook, respirology physician and deputy editor at the Canadian Medical Association Journal (CMAJ), recently wrote in an editorial, “e-cigarettes appear to cause a wide variety of different lung pathologies and clinical illnesses. It is therefore very unlikely that any single compound, contaminant or e-liquid brand is responsible for all of them.”
Evidence from Canada supports this statement. So far, of the 14 reported cases of EVALI, seven people have self-reported vaping only nicotine. One of these patients developed bronchiolitis obliterans, or ‘popcorn lung’, which is thought to be due to the specific flavouring agent use. In the UK, a woman developed lung injury from e-cigarette associated heavy metal inhalation (cobalt).
The more insidious harm: youth nicotine addiction
While the risk of EVALI is well represented in the media, Richard Miech, researcher and professor at the University of Michigan, believes that perhaps the most important risk of e-cigarettes is nicotine addiction. Miech has been studying youth substance use for over two decades.
“Just when it looked like the US had finally figured out a solution to keep the tobacco industry from hooking kids on nicotine and making lifelong customers, along comes vaping,” he says. “If people don’t start smoking by age 18 or so, it is highly unlikely they will ever smoke, in part because the developing teen brain is more susceptible to addiction.”
Miech and colleagues have recently completed population estimates displaying a rapid increase in youth vaping. “Teen vaping prevalence is now endemic, with our project documenting that one in four US 12th graders vaped nicotine in the past 30 days in 2019,” he says. The same is true in Canada, with more than 20% of high schoolers trying it at least once.
One specific type of e-cigarette – JUUL – accounts for almost 80% of all e-cigarette sales in Canada. In addition to being highly marketed towards adolescents, JUUL contains three times more nicotine per cartridge than the allowable limit of e-cigarettes in Europe and causes higher blood nicotine levels than other e-cigarettes. Though JUUL has stated that this is to provide the best nicotine replacement device for smokers, Robert Schwartz, tobacco researcher at the University of Toronto, questions this logic. “There is no reason why anyone needs that quantity of nicotine. From our studies [on cigarette users], you can go much lower to satisfy cravings.”
Schwartz says there is cause to be concerned about the high nicotine content. “For young people, nicotine is highly addictive. It’s as addictive as heroin. And there are some indications that e-cigarettes may, in some instances, bring about addiction faster than smoking,” he says.
In contrast to older adults, most adolescents who use e-cigarettes have never used nicotine or tobacco products previously. Recent Canadian estimates have found that 15% of current e-cigarette users had never smoked before – of these never smokers, 58% were youth aged 15 to 19. Miech and others have shown that e-cigarette users are at a higher risk of going on to smoke combustible cigarettes than those who don’t vape.
When surveyed, the most frequently reported reason for using e-cigarettes among adolescents is that they are available in flavours they like. Youth also may be unaware of potential harms. Data from the Florida Youth Tobacco Survey showed that 50% of adolescents thought there were no risks associated with e-cigarette use, and 67% thought that they weren’t addictive.
Public health officials in the UK, where regulations on advertising e-cigarettes are stricter, believe that the combination of marketing and nicotine content are responsible for the discrepancy in youth vaping rates between the UK and North America. By the most recent estimates, only 6% of UK adolescents had tried e-cigarettes, and less than 3% were regular users. This is compared to roughly 25% trying e-cigarettes and 10% using regularly in North America.
Other potential risks of vaping
While the evidence is not definitive, some studies suggest that nicotine use in adolescence may have an impact on cognitive development and the risk of developing a future substance use disorder. Observational studies have suggested that e-cigarettes are associated with a small but significantly increased risk of heart attacks. And more recently, the US Population Assessment of Tobacco and Health has shown that e-cigarette use is associated with an increased risk of developing lung disease (such as COPD and asthma) after just three years.
But many of the risks to current e-cigarette users simply aren’t known. The main components, including propylene glycol and flavouring additives, need to demonstrate safety when eaten to obtain approval, but do not need to demonstrate safety when inhaled. Furthermore, the lack of regulatory oversight by Health Canada and the FDA results in the availability of products that may not contain exactly what is on the ingredient label.
The recent rise in cases of acute lung injury has led many, including Gupta, to wonder what other harms may soon be revealed. “Will it be emphysema, will it be cancers, will it be cardiovascular disease? I don’t want to find out by doing this natural experiment on our population,” he says.
And for Schwartz, the takeaway is clear. “There is enough evidence to say that if you aren’t a smoker, you shouldn’t go anywhere near these things.”
Global policy measures
The global response to e-cigarettes has been varied, including promotion in the UK, and bans in Australia, Japan and Singapore. In North America, we have not yet taken decisive action for or against e-cigarettes, but many policies have been proposed.
The most popular, and most controversial, has been a proposal to eliminate the sale of flavoured e-cigarettes, given that this is the leading factor for youth e-cigarette use. Flavoured products are banned in Michigan, Rhode Island, Washington, Oregon and Montana, and Massachusetts temporarily banned all e-cigarette sales in late 2019. Many are calling for a more immediate and sweeping public health strategy to curb teen vaping.
Nova Scotia was the first Canadian province to ban the sale of flavoured e-cigarettes, which will take effect by April 2020, and Ontario Health Minister, Christine Elliott, has stated that she is considering the same action in Ontario.
Other efforts have included restrictions on advertising, which have been used effectively in the UK. In Canada, Schwartz comments, “the federal government allowed essentially all forms of advertising and promotion, and the companies, which are owned or partially owned by tobacco companies, are aggressively out there trying to get every possible person that they can, to use their products.”
Under the Canadian federal Tobacco and Vaping Products Act and the Non-smokers’ Health Act, the minimum age to buy any tobacco product is 18. Eight provinces, including Ontario, have adopted provincial e-cigarette legislation. “Starting January 2020, the promotion of vapour products [will be restricted to] specialty vape stores and cannabis retail stores, which are only open to people aged 19 and over,” Elliott said in a written statement to Healthy Debate.
But given the high prevalence of vaping in middle and high-school students, many question how effective this legislation is.
In addition to restrictions on flavouring, advertising and sales to youth, Schwartz also urges the government of Canada to disseminate clear and strong messaging discouraging the use of e-cigarettes.
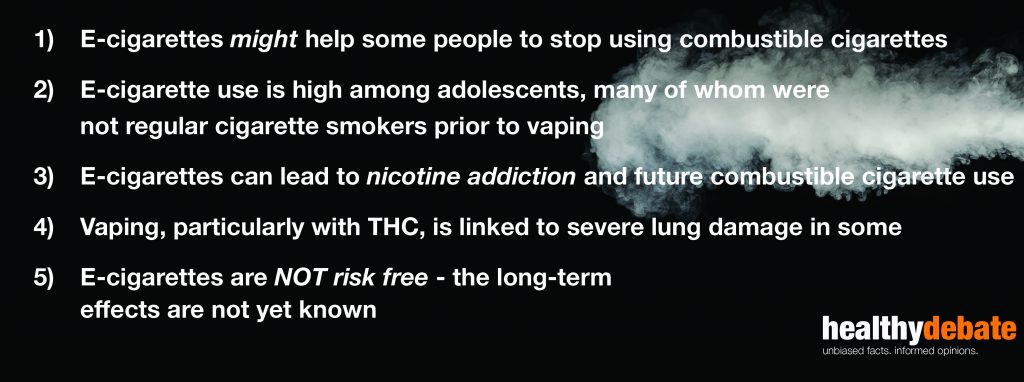
Five important takeaways
While there remain many unknowns, there are a few things we can say about e-cigarettes with confidence:
Global cigarette smoking is an important problem, as is preventing youth nicotine addiction. And while e-cigarettes may have a role to play in future efforts towards smoking cessation, the reality is that we don’t currently have enough evidence to confirm that they are a safer alternative.
And the potential of harm reduction for some is not enough to justify exposing millions of youth to nicotine and unknown long-term risk.
Gupta warns, “cigarette smoking was [also] initially promoted as harm reduction for people using chewing tobacco, which we knew caused oral cancer, and was doctor recommended… We don’t want to see history repeat itself.”
This piece was edited by Salima Shariff, Chika Oriuwa & Drew Cumpson


The comments section is closed.
I agree with the fact they may not be risk free. However, from my understanding, they are far safer than the use of traditional cigarettes. Public Health England have stated they are 95% safer. Nicotine, whilst it is addictive, isn’t much worse than caffeine.
Ref
https://dragonvapour.com/
After years of working in construction and smoking cigarettes,I was diagnosed with COPD and pulmonary fibrosis. As my illness progressed, I found myself relying on supplemental oxygen around the clock. Even getting out of bed became a challenge.My doctors and specialists recommended a lung transplant, but after researching the pros and cons of such a drastic procedure, I decided to try something less invasive. I contacted multivitamin herbal cure cape town for organic natural treatment you can search for them on google. Following the COPD and pulmonary fibrosis herbal treatment procedure , my lung function has improved dramatically after my first four weeks of the herbal formula .My quality of life has gotten a lot better. I was amazed that I could breathe without any dead air. I no longer need oxygen and look forward to continued improvement because a specialist told me already I have a 97% chance of getting my condition totally due to the herbal treatment effectiveness . If you or someone you love has COPD, pulmonary fibrosis or another chronic lung disease, and would like to see improvements like mine they even guarantee me totally cure once the treatment is done , their website multivitamincare , org they will put you through on the herbal process.
Amazing content all the assumptions are mention in this blog. Vaping is the best way to quit or reduce the habit of smoking . If you are looking for good E-Cigarettes please click on the links you will get a good quality of vapes: https://www.ibreathe.co.uk/
We thank Healthy Debate and Colacci and his colleagues for their timely important contribution to e-cigarette prevention (1). Even though e cigarette industry is aggressively advocating and promoting nicotine vaping as a safest tobacco cessation tool “few adolescents try to quit smoking using any sort of cessation aid or professional intervention and the efficacy of e-cigarettes in improving smoking cessation in youth is equivocal”(2).
We thank Healthy Debate for continued advocacy in support of the adolescent health and well-being (1). Getting adolescents involved in this prevention program is crucial and the key to success (3, 4, 5). We urge Canadian Physician Organizations to take a leadership role in a Canada-wide comprehensive school awareness and prevention program. We could perhaps tailor e-cigarette prevention programs similar to the old combustible cigarette prevention education programs (3). We need an effective social media campaign to enhance adolescents’ knowledge about the ingredients in e-cigarettes, their potential adverse effects and the known health hazards of prolonged use and misuse. There also needs to be a strong public education and awareness campaign to counter common myths and misconceptions (e.g., like e-cigarettes are a safer therapeutic tool) (3).
It is urgently needed to introduce a brief online training module as part of continuing medical education (CME) on how to use every opportunity of “teachable moments in the respective clinical practice”. “Teachable moments” has been commonly described as an opportunity to facilitate education and patient behavior change. Every clinical visits potentially could be an instance of a ‘‘teachable moment’’ to help educate young patients with vaping related potential serious adverse events and motivate behavioral change. It is important that the training module should develop in consultation with the Canadian Medical Association, Canadian Pediatric Society and the College of Family Physicians Canada. It is also important to involve adolescents in the process (4). Educational tool may be designed taking in to consideration of the context of interactive clinical scenarios.
REFERENCES:
(1). Colacci M. E-cigarettes and vaping: the bad, the good, and the unknown? Healthy Debate Jan. 2020- http://healthydebate.ca/2020/01/topic/a-deep-dive-into-vaping
(2). Wolfenden L, Stockings E, Yoong SL. Regulating e-cigarettes in Australia: implications for tobacco use among young people. Med J Aust 2017; 208 (1):1. || doi: 10.5694/mja17.00787
(3). Bandara NA. Would e-cigarette regulation alone improve adolescents’ health? CMAJ. 2016 Oct 18;188(15):1106.
(4). Bandara NA. The consultation of youth in the public health care policy-making process. Can J Public Health. 2016 Aug 15;107(2):e216. doi: 10.17269/cjph.107.5446.
(5). Bandara NA, Seneviratne M. Adolescents’ Electronic Cigarette Use. Pediatrics. 2019 Jan;143(1). pii: e20183151. doi: 10.1542/peds.2018-3151.
Aki Nilanga Bandara
Founding Chair-Global coalition to empower adolescent and youth on harmful therapeutic interventions to prevent combustible tobacco use.
Instructor, Faculty of Land and Food System, University of British Columbia, British Columbia, Canada, 2357 Main Mall, Vancouver, BC V6T 1Z4 Canada.
Mehara Seneviratne
Coordinator-Global coalition to empower adolescent and youth on harmful therapeutic interventions to prevent combustible tobacco use.
Dr. Vahid Mehrnoush
Senior Advisor-Global coalition to empower adolescent and youth on harmful therapeutic interventions to prevent combustible tobacco use.
Postdoctoral research fellow, Section of Trauma, Acute Care, and Global Surgery, Vancouver General Hospital, University of British Columbia, Vancouver, BC