Despite more and more women entering the medical field, gender inequities in culture and lifestyle demands have led women to still be underrepresented in some specialties.
The Canadian Residency Matching Service (CaRMS) takes place annually and is where graduating medical students apply for and match to their medical specialty of choice, such as internal medicine, family medicine, dermatology and neurology, along with surgical specialties such as urology, otolaryngology and general surgery.
Gender differences in specialty choice has long been a topic of interest to the medical community, especially since research has demonstrated female physicians in both surgical and medical specialties have better patient outcomes than their male counterparts. Some known factors that influence students’ choices include future job prospects, lifestyle and patient population; however, it has also been established that personal factors such as personality fit and gender equity within the specialty are prominent motivators.
Compared with 20 years ago, more women are entering the medical field; indeed, the majority of graduating doctors in Canada are female.
Since the 1980s, researchers have reviewed the representation of women in medical specialties and multiple studies have demonstrated that women have been overrepresented in primary care specialties like family medicine and pediatrics while underrepresented in surgical specialties. As the proportion of women in medicine has changed since 1980, how has this affected the gender balance in individual specialties?
In March 2020, nearly 3,000 medical students matched to residency positions across Canada. Approximately 56 per cent of these applicants were women. While women still comprised the majority of family medicine and pediatrics applicants, women also made up the majority of applicants for general surgery, internal medicine, plastic surgery, obstetrics and gynecology, and vascular surgery. In the United States as well, a majority of applicants in general surgery were women. Though this seems like positive progress, is it actually?
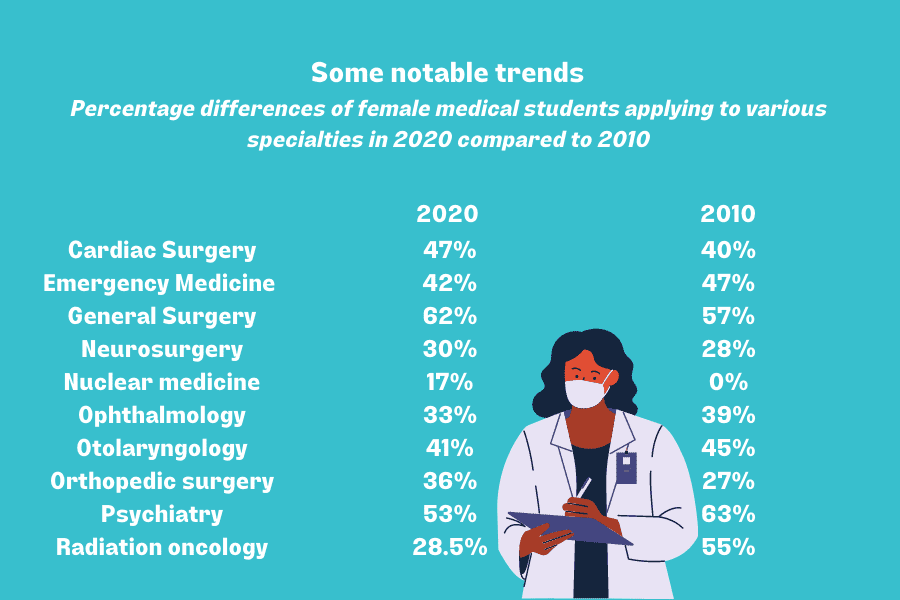
Comparisons to Canadian residency matching data from 2010 (with 58 per cent female applicants) show some notable shifts by 2020, but largely, the gross distribution of applicants by gender and specialty remain similar.
Differences include an increased proportion of male applicants to primary care specialties such as family medicine and pediatrics as well as psychiatry. Additionally, more women applied for general surgery than in 2010.
But while the numbers themselves are interesting, they fail to tell the whole story.
We have long known that there are consistent gender differences in factors considered when selecting specialty as well as differences in how men and women practice medicine. Women are known to more highly value lifestyle factors, such as schedule flexibility, fewer work hours and the ability to have children during residency without stigma, whereas men are more motivated by status, income and career or promotion expectancies. Additionally, women gravitate toward specialties with greater interpersonal and communicative approaches.
While these factors may explain some of the immutable discrepancies between male and female applicants, more recent data demonstrates that for surgical specialties specifically, women are not deterred by the lifestyle or workload, but the perceived stereotypes about “surgical personality” and surgery culture. Additionally, this same study demonstrated that lifestyle is a deterrent for surgery for both men and women, therefore it is not just a “women’s” issue.
These results suggest there are areas where residency programs can improve in attracting more female applicants:
1) Reducing stigma surrounding childbirth during residency – as the medical student population increases in age, having children during residency is more common. Reducing stigma and implementing more parent-friendly policies can increase the attractiveness of high-intensity residency programs to female candidates;
2) Female representation and mentorship – people aspire to what they can see, and if they can relate to a mentor in a specialty they may not have originally considered, it may influence their choices;
3) Accountability and recognition of discrimination in the workplace resulting in a shift in program culture – institutions and individuals must hold people accountable when there are instances of harassment or discrimination as this may influence specialty and residency program choices. This will allow applicants to feel safer in their working environment and like they belong.
Gender differences in medical specialty choice still exist today. While female students make up the majority of applicants to surgical specialties such as general surgery and obstetrics, they are still also overrepresented in primary care specialties such as family medicine and pediatrics.
Imbalances exist in programs such as ophthalmology, emergency medicine, nuclear medicine, radiation oncology, orthopedic surgery, neurosurgery, otolaryngology, diagnostic radiology and urology, with the male-to-female ratios of many of these fields having worsened over the past 10 years. Increased and proportionate female representation in all specialties is important given that female physicians tend to have better patient outcomes and increased representation can serve to change the culture of the specialty as a whole.


The comments section is closed.
My comment: Palliative Medicine.