In this series, AMS Healthcare addresses the challenges facing healthcare today – particularly in light of the COVID-19 pandemic. The AMS Community promotes compassionate care, development of the leadership needed to realize the promise of technology and the understanding of how our medical history influences the future of our healthcare. A new piece will be posted every Friday on Healthy Debate.
Our skies have grown more silent. The air we breathe, cleaner by the day. Thunderbirds that once roared overhead lie sleeping, grounded in their hangars.
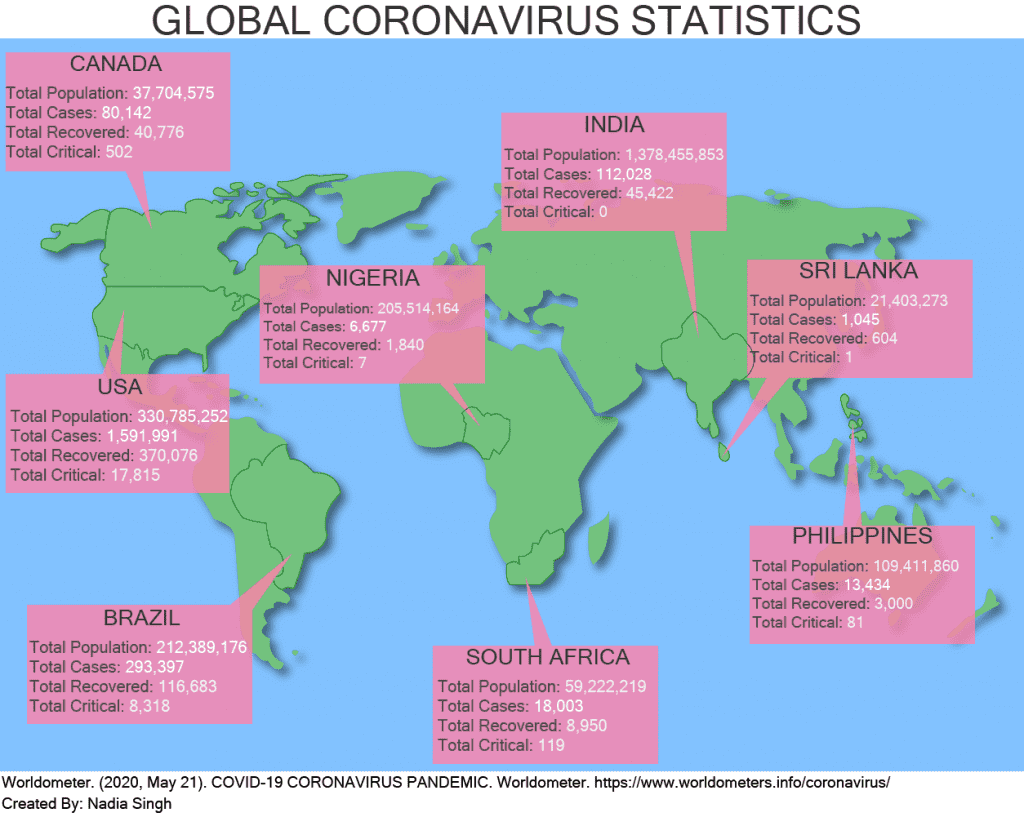
The once wondrous aviation technology bears responsibility for rapidly shifting the COVID-19 virus from a localized epidemic in China into a global pandemic. In some parts of the world, there is no hope of jobs or social assistance during and after the pandemic. Even if those of us that live here become sick and can make our way to a hospital, there will be no ventilator if we need it. In the Brazilian favelas, the Indian slums and the South African informal settlements, there can be no six feet of physical distancing where a neighbour’s house is crammed next door.
In countries with resources, technology is being harnessed to both forecast healthcare needs and to prevent further spread of COVID-19. Artificial intelligence is used to predict surges in emergency rooms, where these new technologies are met with “optimism and potential.” Virtual care is suddenly a possibility for health professionals to connect safely with patients. Apple and Google have announced partnerships to use Bluetooth technology for contact tracing.
These technologies may save lives in well-resourced areas but are inaccessible in under-resourced nations.
The pandemic has exacerbated the fight for global resources. Countries with underdeveloped public health systems will need to rely on support from the World Health Organization yet the United States has moved to defund it. The COVID-19 pandemic is widening social inequities at local and global scales.
History indicates that technology is not neutral, that it changes how we interact with the world around us. Closing the health technology gap between privileged nations and under-resourced nations will be the true test of compassion and equity for us.
In the echo of the United Nations’ call for technologically advanced nations to reach out to Africa, we wonder: Will the privileged retreat behind science and technology known to be inequitable or will they reach out? How effective will we be at turning our attention from the technologies of economic growth, development and self-preservation to technologies for compassionate connection and equitable opportunities for survival?
While politicians sprout promises that a COVID vaccine could be available in a year, history reminds us that this would be a technologically unprecedented, even revolutionary, event. For many, the primary concern is who will have access to the vaccine and by what means? Referencing history, we must conclude that in a global clamour, economics will determine access. Banting, Best and Collip sold the patent rights for insulin to the University of Toronto for $1. A century later, insulin has moved from being a public good to a drug that is inaccessible to thousands because of its cost. A COVID-19 vaccine must avoid this fate. If the global bidding wars and scramble for personal protective equipment are harbingers, access to a COVID-19 vaccine will test the health systems of countries that provide vaccines as public health initiatives. Vaccine developers will be intent on recouping costs and making profits.
Under-resourced nations harbour no delusions, remembering the “drug wars” for affordable access to antiretrovirals in the AIDS pandemic. India successfully challenged patents to manufacture antiretroviral generics and the Treatment Action Campaign in South Africa fought for free antiretrovirals. Will time allow for this kind of activism before thousands die again, before technology is harnessed for compassion rather than profit?
COVID-19 reveals how the intersection between technology and compassion can advance equity in the novel COVID-19 world we abruptly share. When human cacophony resumes, will our compassion for one another be compromised? Will the technological “solutions,” the exchanges of medical equipment, vaccines and emergency funding we have negotiated enable the global distribution of compassionate care or will we have benefited only the well resourced, leaving entire communities, if not entire nations, behind?
As life has changed on a dime, and those who are fortunate enough to have a home shelter in place, we must be mindful that the technology that guides our leaders and healthcare providers must be equitable. Without equity, compassionate care will be enacted only for the lucky few.
*With acknowledgement to our book chapter collaborators, Arno Kumagai, Lisa Richardson and Ayelet Kuper. The ideas in this blog are further explored in the upcoming book Without Compassion There is no Healthcare from McGill/Queen’s University Press.


The comments section is closed.