This series is a deep dive into the lives and working conditions of health-care professionals across Canada. It includes six profiles that explore the challenges, triumphs and priorities not only of our the health-care system as a whole, but of the workers who support it.
Feature by Wendy Glauser
Profiles by Maddi Dellplain, Sahil Gupta, Nicole Naimer and Maria Raveendran
Emergency departments are closing across the country. Wait times in those still open frequently surpass 20 hours. An unprecedented number of people are being cared for in hallways and spaces not designed for care as they wait for specialists or procedures. Frail elders are waiting months in loud and uncomfortable hospital rooms for a long-term care spot. About one in five Canadians are without a family doctor.
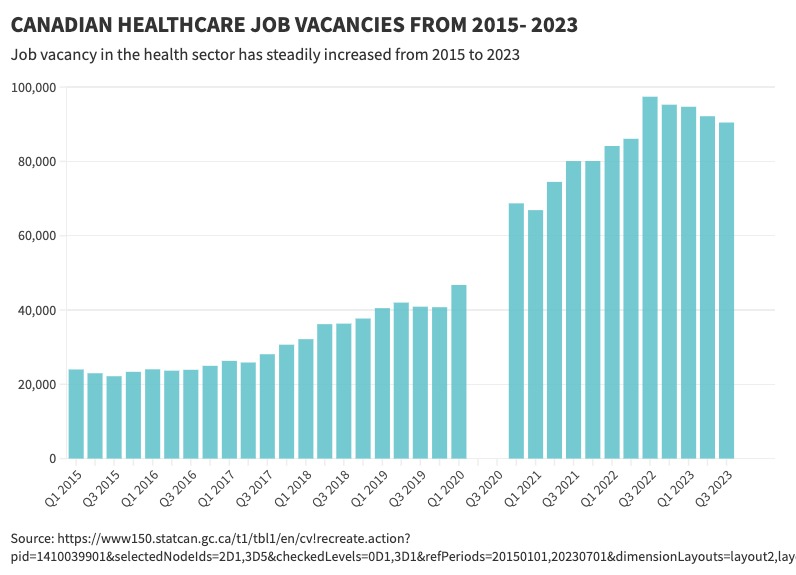
It’s not a lack of hospital beds or buildings that’s driving this crisis. Our health-care systems are collapsing because there aren’t enough people willing to work in them. As Prince Edward Island Health Minister Mark McLane said last fall, when Canada’s provincial health ministers gathered in Charlottetown, the top three issues facing our health systems “are staffing, staffing and staffing.” The number of vacant health-care positions are now almost 92,000, up from about 22,500 in 2015, according to Statistics Canada.
‘Nurses are not a commodity. We are human’
Kari, a registered nurse in Toronto. Read her story.
Pay is a major factor explaining why people are leaving health-care jobs or choosing not to enter the professions in the first place. Doug Allan, a health researcher with the Canadian Union of Public Employees in Ontario, says the gap between salaries for health-care jobs versus non-health-care jobs has shrunk in the past decade. Statistics Canada data shows that in 2015, the average hourly wage of people working in Canadian hospitals was 51 per cent above the all-industry average, which includes well-paid office jobs but is weighed down by low-paid and non-unionized service-sector jobs. In 2023, hospital wages were just 19 per cent above that all-industry average in Ontario. This shrinking gap demonstrates “there are more opportunities in other (non-health care) industries that are more attractive,” says Allan. “We have people in this sector rethinking their career choices.”
Wage suppression legislation put into place just before the pandemic certainly didn’t help. Ontario’s Bill 124 capped public sector employees at 1 per cent yearly increases (while inflation grew to 9 per cent). Alberta and Manitoba also suppressed health workers’ wages.
“The insult that you would have people risk their lives in this extraordinary pandemic and then also have wage suppression legislation at the same time … it was like a fork in the eye to people who, remember, were sleeping in garages, were not going home to their families,” says Natalie Mehra, executive director of the Ontario Health Coalition, recalling the extraordinary measures that many health-care workers took to avoid passing a deadly virus to family members.
Although Ontario’s Bill 124 was ruled unconstitutional and retroactive pay awarded, the damage had been done. Pandemic pressures and wage caps had already driven seasoned health workers not just in Ontario but across the country to retire early, explains Carrie Fletcher, a lecturer at University of Toronto’s Institute of Health Policy, Management and Evaluation. “There was a mass exodus of seasoned clinicians, seasoned nurses, social workers, occupational therapists and physical therapists.”
‘You just go to the bathroom and cry it out.’
Paula, a licensed practical nurse in Red Deer. Read her story.
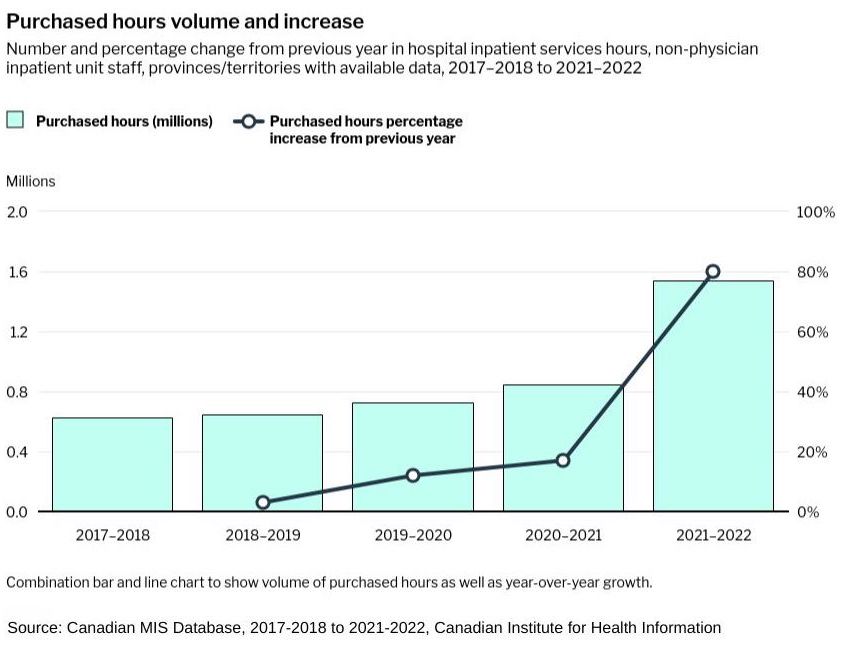
Governments hired private agencies to fill the gaps – agencies that paid nurses more than $100 an hour, in some cases, while charging hospitals up to $300 an hour per nurse, as a Globe and Mail investigation revealed. The stop-gap measure made shortages worse as nurses, lab techs, health-care aides, respiratory therapists and others chose flexible agency work over full-time permanent positions.
“Just over two years ago, we did not have one agency nurse in New Brunswick,” says Maria Richard, vice president of the New Brunswick Nurses Union. But from the summer of 2022 to 2023, New Brunswick’s government paid more than $50 million to private staffing agencies, the Globe found. Working alongside nurses that were making double or triple their pay was another gut-punch for those on staff. As Allan explains, health workers are expected to train agency workers, who may not be familiar with the care protocols and electronic systems. “It’s extra work for the rest of staff, and then there’s the irritating fact that the [agency health workers] they’re training are actually getting paid more than they are.”
There are other demoralizing discrepancies, too.
‘This used to be a job that could sustain you … it’s not anymore.’
Kris Vickberg, a porter in Vancouver. Read his story.
Many family doctors earn far less than what other specialists make, which explains why the number of physicians interested in family medicine has been steadily decreasing over the years. There’s also a large pay gap between registered nurses (RNs), who have four years of university, and registered/licensed practical nurses (RPNs/LPNs), who have two years of post-secondary education but whose duties are expanding. Paula*, a licensed practical nurse in Alberta, says LPNs are increasingly being asked to get on-the-job-training and take on tasks that previously required an RN designation – without any commensurate pay increase. This is happening across the country, too.
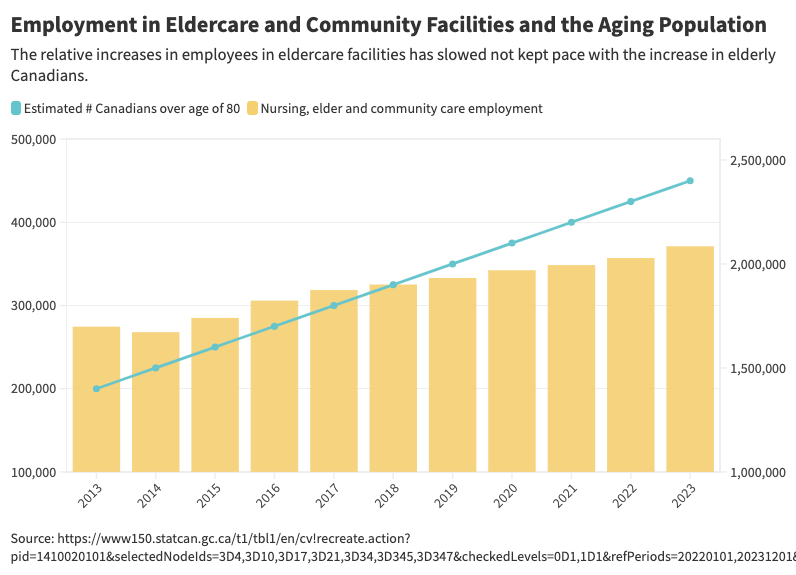
Meanwhile, the workload and stress of health-care jobs have soared. Nurses, personal support workers, porters and others have no choice but to work at an exhausting pace every time they’re short-staffed. A common theme among the health workers we profiled for this series is that they’re required to work short-staffed more often than ever, not only because of vacant positions, but also because of a high rate of absenteeism from injury and overwork. This is especially the case in long-term care, which became infamous during the pandemic for a lack of oversight and standards across a fragmented patchwork of private and public ownership.
Bonnie Gostola, a vice president of the Alberta Union of Public Employees, points out that long-term care homes “don’t have a mandate to make sure that they actually fill positions when they’re vacant, or that they actually fill sick calls when they’re made.” The veteran care aide says that 20 years ago, “you would have never heard of a long-term care facility going shorthanded. If somebody called in sick, there was always a replacement. That is not happening now.”
The heavy workload “was the major issue for the health-care workforce leading into the pandemic,” says Mehra of the Ontario Health Coalition. Now, that problem is “much worse than it was before the pandemic.”
With a higher workload comes more injury. People get hurt doing patient lifts in the wrong way because they’re rushed, Mehra explains, or a care worker lifts a patient by themselves when protocol requires a two-person lift, “because there are no other staffers around to help them.” The latest available data from the Canadian Institute of Health Information (CIHI) reported a 17 per cent year-over-year increase in sick days among health workers from 2021-2022, compared to 3 per cent average increases in the four previous years.
Health-care staff not only have to work harder because of shortages, they also have to work longer. Statistics Canada reports that, on average, health-care workers put in 6.7 hours of overtime per week in 2019, increasing to 8.6 per week in 2022, the most recent figure available. Overtime is a double-edged sword. Charlotte, a care aide working in long-term care in Saskatchewan included in this series, is paid 1.5 or 2 times her hourly rate when she works overtime, depending on how long her overtime shift lasts. Working 60-hour weeks has helped her keep up with the fast-rising cost of living. But health workers don’t always have a choice of when or whether to work overtime, and being mandated to work four more hours, on top of a physically and emotionally intensive eight-hour shift, is a recipe for burnout.
‘We shouldn’t have to work 2 or 3 jobs to survive.’
Lisa Allen, a personal care attendant in St. John. Read her story.
Over the past winter holidays, Richard says the situation was so dire in her province that nurses were mandated to work in emergency departments. “These nurses were telling us, ‘I’m not trained to work in emerg. I’m working above my scope of practice and it’s not safe.’ ”
Last summer, Richard says, a New Brunswick nurse reported that she had to work 36 hours straight because her hospital floor was too understaffed to let her go home. Paula in Alberta described how being short-staffed increases patient frustration and worsens the abuse frontline workers’ experience. An investigation by Carleton’s journalism school found that assaults against health workers increased by 25 per cent from 2020 to 2022.
Many of the people we talked to say employers exploit caregivers’ compassion for their patients – health workers do extra work outside of their scope, rush to the next patient and stay late because they know patients will suffer if they don’t. “Caregivers aren’t really prone to wanting to walk away from their clients. It’s something that employers prey upon,” says Gostola.
But sometimes, try as they might, it’s impossible for health workers to get to all the patients who need them, or provide the level of care they know patients deserve. “We’re hearing ‘If it was my dad or mom in that bed, I would be totally disgusted by the care I was able to give today,’ ” says Richard. “That’s why we talk about the ethical and moral dilemma that nurses are dealing with, because when you’re supposed to have five nurses on the floor, and you arrive, and there’s only one or two, you have to cut corners somewhere. That’s the reality.”
"Choosing to a job that pays less, because you enjoy it, only goes so far."
Vanessa, a family doctor in Winnipeg. Read her story.
Mehra says she has heard stories of long-term care homes being so short-staffed that “they don’t get their baths. Nobody gets their teeth brushed. They don’t get dressed properly.”
The situation is bleak, but the health workers and labour experts we spoke to see ways forward. This year, British Columbia became the first province to set minimum nurse-to-patient ratios, including one-to-four in general medical and surgical wards and one-to-two in high-acuity units. (The province is working out long-term care ratios as well).
Mandatory minimum ratios would go a long way to reduce burnout, as well as the physical and moral injuries that health workers experience. Erin Ariss, president of the Ontario Nurses Association, whose organization unsuccessfully called for similar ratios last year, says in Ontario, nurses in short-staffed general units are reporting having to care for up to 12 patients at once. Mandatory ratios also would require long-term care homes to be proactive about filling in sick calls and hiring more permanent staff. Of course, mandatory minimums require an adequate workforce to meet them, so they have to come alongside increased funding for training spots and attractive salaries and schedules. On top of mandatory ratios, Richard would like to see rules in place so that nurses cannot work beyond a certain number of hours in a row, for patient and health worker safety. Truckers and pilots have limits on how much they are allowed to drive or fly without resting, she points out. “Why aren’t there any regulations for health-care workers?”
Hospitals can find ways to bring in flexibility in scheduling. Kari says when her hospital refused to meaningfully change her schedule – a gruelling four 12-hour shifts in a row, two nights and two days – she moved to agency work so she could pick her shifts and see her children more. “This generation, they want agency. They want flexibility and work-life balance,” says Fletcher. Adds Ariss: “We can work through our bargaining processes to negotiate scheduling language in our collective agreements that allows for flexibility, there just needs to be a willingness [on the employer’s part].”
‘These are absolutely the most vulnerable workers.’
Charlotte, a continuing care assistant in Saskatoon. Read her story.
Increasing pay to nurses on staff would also make agencies far less alluring. Fletcher says her organization started paying double-time to staff nurses for overtime instead of time and a half – avoiding, in many cases, having to pay agencies exorbitant amounts to fill in gaps, and the morale issues that come with that.
Health workers spoke about better management support – having staff on the floor to ensure that workload is fairly distributed – and on-the-job mentoring, training and promotion opportunities. With the loss of veteran health workers, many nurses say they don’t have someone to turn to with questions or to watch them when they do a procedure on the job for the first time.
“Some of the nurses that we’ve lost … we might be able to convince them to come back and be mentors,” says Richard, explaining that the nurses would need to be properly compensated and know they aren’t coming to disastrously understaffed facilities.
There are already examples that are working. B.C.’s recent increase in pay for family physicians upped the number of physicians providing comprehensive family medicine by 16 per cent. The province has also brought in a program that pays for workers’ education to become health-care aides while they are paid for restocking, meal-time support and other duties in hospitals and long-term care homes. Many Atlantic provinces are offering retention programs for nurses, and last year, Manitoba invested $500 million in training Canadian and international health-care workers. In Nova Scotia, almost 150 nurses who had retired or taken up casual or agency work signed up for permanent positions when the province offered a $10,000 signing bonus.
Many of the health workers spoke through tears about relationships they’ve had with their patients, and what an honour it is to be there for them, to help them through their fear and pain, to learn about their lives, to cheer on their successes. But everyone reaches a breaking point. And too many health workers are close to theirs.
As Richard puts it, “We need to know there’s a light at the end of the tunnel.”
* Names have been changed at their request.